The Functional Assessment Staging Tool (FAST) is a dependable method often used to assess the current state of dementia in patients. It offers a thorough and effective evaluation of functional abilities and the potential for decline over time. This makes it an essential resource for healthcare professionals, caregivers, and family members to monitor the capabilities of dementia patients.
What is the FAST Dementia Rating Scale?

The Functional Assessment Staging Scale is a way to determine if your loved one has dementia. Dr. Reisberg developed FAST in 1982 as a tool to define and rate all types of dementia. The FAST scale has seven stages:
- No cognitive or functional impairment
- Early functional changes
- Mild functional decline
- Moderate functional losses
- Moderately severe loss of function
- Severely reduced functional capacity
- Total dependence
mobility, and feeding. Families worried about Alzheimer’s and other dementias can use the FAST scale to gauge the extent of cognitive decline in their loved ones. Knowing the person’s functional level helps determine their specific care needs. It also allows caregivers to track changes in a patient’s functional status as early as possible with accurate results.
Understanding the Fast Score for Dementia

The FAST Scale categorizes the progression of dementia based on the person’s ability to perform daily tasks and activities. The scale consists of seven stages, with higher stages, indicating more significant impairment.
Here is a further breakdown of the stages:
Stages of the FAST Dementia Scale
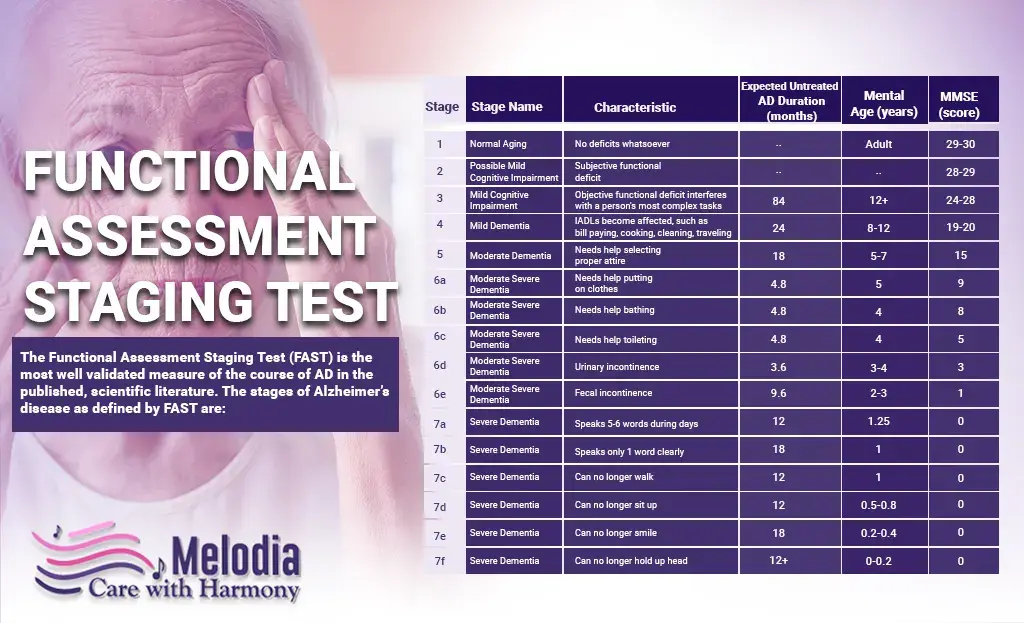
Here is a breakdown of the stages of the FAST Dementia Scale:
1- No subjective or objective difficulty
2- Complains of forgetting where things are; has trouble finding words
3- Decreased job performance noticed by coworkers; traveling to new places is hard; reduced organizational skills
4- Difficulty with complex tasks (e.g., planning a dinner, managing finances, shopping)
Needs help choosing proper clothing for the day, season, or occasion
6a. Trouble dressing properly without help (e.g., mismatched clothes, difficulty with buttons)
6b. Needs help with bathing (e.g., adjusting bath water)
6c. Problems with toileting (e.g., forgetting to flush, improper wiping)
6d. Occasional or frequent urinary incontinence
6e. Occasional or frequent fecal incontinence
7a. Can only speak six or fewer words on an average day or during an interview
7b. Speech limited to one word, repeated often
7c. Cannot walk without assistance
7d. Cannot sit up independently
7e. Cannot smile
7f. Cannot hold up head independently
Duration of Each Stage

Alzheimer’s disease progresses clearly through the FAST scale, with all stages typically occurring in order, though there may be some overlap. This progression is not always seen in other dementias, where patients might skip stages. According to the Alzheimer’s Association, a person with Alzheimer’s lives an average of four to eight years after diagnosis but can live up to 20 years. Before showing symptoms, the brain can undergo years of subtle changes known as preclinical Alzheimer’s disease.
The below table provides an overview of the stages of dementia, detailing the diagnosis, the stage of cognitive decline, the signs and symptoms associated with each stage, and the expected duration of each stage.
| Diagnosis Stage | Signs and Symptoms | Expected Duration of Stage |
|---|---|---|
| No Dementia Stage 1: No Cognitive Decline |
|
N/A |
| No Dementia Stage 2: Very Mild Cognitive Decline |
|
Unknown |
| No Dementia Stage 3: Mild Cognitive Decline |
|
Typically lasts between 2 and 7 years |
| Early-stage Stage 4: Moderate Cognitive Decline |
|
Generally lasts about 2 years |
| Mid-Stage Stage 5: Moderately Severe Cognitive Decline |
|
Typically lasts around 1.5 years |
| Mid-Stage Stage 6: Severe Cognitive Decline (Middle Dementia) |
|
Generally lasts about 2.5 years |
| Late-Stage Stage 7: Very Severe Cognitive Decline (Late Dementia) |
|
Typically lasts between 1.5 and 2.5 years |
The FAST Scale: Hospice Care Criteria

Alzheimer’s patients receiving palliative care are usually in stage seven. At this stage, they have significant difficulties with communication and independent movement. Many Alzheimer’s patients also have other illnesses, such as coronary heart disease. Doctors consider all these factors when deciding if a patient qualifies for hospice care. Alzheimer’s patients typically enter hospice care during the final stages of the disease. At this point, they usually:
- Need help with daily activities and personal care around the clock
- Are unaware of recent events and surroundings
- Have changes in physical abilities, including trouble walking, sitting, and swallowing
- Have more difficulty communicating
- Are prone to infections, especially pneumonia
In the final stages, patients struggle to respond to their environment, talk, and control their movements. They might still say words or phrases, but it can be hard for them to express their pain or needs. As their memory and thinking abilities decline, they might experience significant personality changes and need more help with daily activities.
Utilization of the FAST Score in Hospice Care

In hospice care settings, the FAST Score can help in several ways:
Patient Evaluation: It helps hospice teams assess the current functional status of patients with advanced Alzheimer’s disease. This evaluation guides the creation of personalized care plans to address specific needs and symptoms.
Prognosis: For advanced Alzheimer’s patients, the FAST Score predicts survival. It is crucial in determining if hospice care is appropriate for a patient.
Care Planning: The FAST Score helps tailor care interventions to the needs of patients and their families. The score can help predict the need for specialized care and assistance as the disease progresses.
Communication with Families: The FAST Score helps in discussions with families about the disease progression, treatment options, and prognosis. It helps manage expectations and ensures the patient’s wishes and care goals are respected.
Measuring Outcomes: In hospice care, the FAST Score is used to evaluate the effectiveness of interventions and track changes in functional status over time.
It is important to note that the FAST Score may be used differently in hospice care depending on institution-specific policies, regional practices, and individual patient needs.
Contact Melodia Hospice Care
If a loved one is progressing along the FAST scale, our hospice care team can help you make decisions about their care while they can still provide input. We aim to ensure that these desires are carried out when the time comes. Contact us at 1-888-635-6347 to learn how we can help you and your family navigate and understand the FAST scale as it relates to your loved one’s hospice journey.







